



Why is this product suitable?
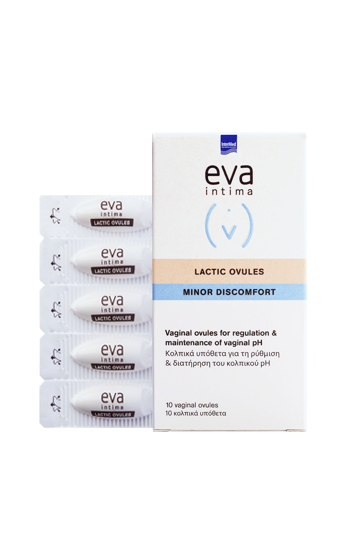
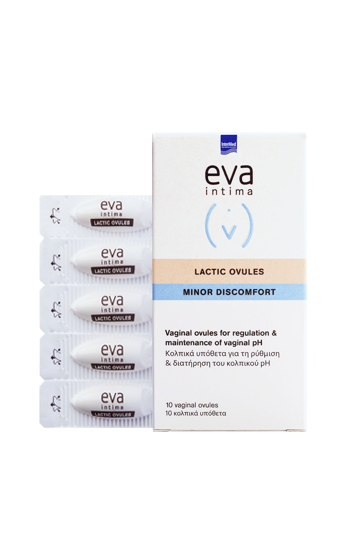
EVA INTIMA® LACTIC OVULES with lactic acid and glycogen is designed to immediately restore the vaginal pH to its normal acidic value while enhancing the normal vaginal flora. At the same time, it relieves symptoms due to its minor disorders such as hypersecretion, itching, irritation & burning, as a result of bacterial infections or other conditions and offers an immediate feeling of relief thanks to the chamomile and aloe extracts it contains.

Balancing-Relief

Innovative composition with herbal extracts
How does it work;
It reshapes the vaginal micro-environment at acidic pH values, pleasing to the beneficial lactobacilli while at the same time providing them with the glycogen necessary for their survival.
This action strengthens the local defense mechanisms and reduces the occurrence of minor irritations.
It does not contain medicinal substances, hormones, synthetic colors and fragrances.
How do I use it?
The application is done the night before bedtime.
- In vaginitis, as an adjunct to medication, and after long-term treatment with antibiotics or contraceptives: One application daily for 7 days
- Preventive: One application per week. During menopause, one application every three days.
- After the period, one application a day for three days.
Remove a vaginal suppository with its case from the blister by tearing in the perforated area. Open the case and remove the vaginal suppository by pulling the two flaps opposite the bottom of the case. Insert the vaginal suppository deep into the vagina using the index finger.
WE ARE HERE to answer you
Each question corresponds to a need. That is why it is worth answering it.
What is vaginitis?
Vaginitis is characterized by inflammation of the vaginal mucosa, i.e. the lining that covers the inner surface of the vagina.
What are the symptoms of vaginitis?
The main symptoms of vaginitis, regardless of its etiology, are the presence of pruritus (itching), irritation, burning and excessive secretions of a different texture, smell and color from the normal ones. Pain during sexual intercourse and urination can often coexist.
What are the most common causes of vaginitis?
The most common causes of vaginitis are bacteria and fungi and can often be caused by a lack of estrogen or allergies (e.g. from the use of condoms or other intravaginal products). However, it is not uncommon for inflammation to occur but without finding a specific cause. These cases are characterized as non-specific vaginitis and are usually attributed to hormonal imbalance (common during pregnancy).
How do I know if I have bacterial vaginosis?
Bacterial vaginitis is the most common vaginitis. Symptoms that usually predominate are pruritus (itching), irritation, burning and the appearance of excessive secretions of thin texture, strong odor (fishy) that may intensify after sexual intercourse or period, and has a gray color.
However, special care is required as there are sexually transmitted diseases caused by bacteria such as vaginal trichomonas infection.
In any case, the correct and safe diagnosis and treatment is performed only through the gynecologist after a series of diagnostic tests (colposcopy, vaginal discharge culture, etc.), a practice that is recommended to follow every time you notice changes in the wider area.
How do I know if I have fungal vaginitis?
Fungal vaginitis is the second most common vaginitis. It is not a sexually transmitted disease and cannot be transmitted as fungi are part of the normal flora of the vagina, where they remain normal in low populations. Common causes of their overgrowth that can lead to vaginitis are conditions that lead to a decrease in lactobacilli in the vagina and the predominance of other microorganisms in the area (e.g. after taking antibiotics for any reason, use of inappropriate and strong antiseptic vaginal solutions, etc.).
Symptoms that are usually predominant are intense pruritus (itching), irritation, burning and the appearance of excessive secretions of viscous texture and white color characterized as leukorrhea, without the presence of a characteristic unpleasant odor.
In any case, the correct and safe diagnosis and treatment is performed only through the gynecologist after a series of diagnostic tests (colposcopy, vaginal discharge culture, etc.), a practice that is recommended to follow every time you notice changes in the wider area.
How can I relieve the symptoms of vaginitis?
Depending on the symptoms that concern you there are product options that can relieve you. However, complete relief from the cause of inflammation can not be achieved without first diagnosing it and receiving appropriate treatment from your gynecologist.
In case of bacterial etiology of vaginitis you can combine (scheme for bacterial vaginitis)
In case of fungal etiology of vaginitis you can combine (scheme for fungal vaginitis)
In case of non-specific etiology of vaginitis you can combine (figure for atypical vaginitis)
How can I prevent the appearance of a vaginitis?
The appearance of a vaginitis can be prevented if the normal flora of the area is maintained with the predominance of lactobacilli, the acidic environment of the vagina (pH 3,5-4,5) in the presence of lactic acid and the necessary moisture for the tissues. Securing these factors prevents the development of infections. In case their presence is disturbed, appropriate product options such as probiotics, vaginal pH regulators and hydrating products can help to restore and maintain them and prevent infections.
Indicatively you can combine (scheme for prevention of vaginitis and enhancement of natural balance)
Tips:
- You can adopt the daily intake of probiotics by mouth through special supplements with lactobacilli to easily and naturally strengthen the flora of the vagina
- You can use daily special cleansing fluids for the sensitive area with enhanced composition for protection against microorganisms.
I often get vaginitis shortly after my period. Why is this happening to me? What can I do?
The transition to reproductive age is marked by the periodic appearance of bleeding that lasts for a few days and usually occurs every 24 to 28 days. The presence of blood in the vaginal area -although normal- can lead to minor disorders in the vaginal environment affecting the vaginal pH and the presence of lactobacilli as the blood has a neutral pH. This effect, combined with the fact that blood is an excellent nutrient medium for fungi normally present in the vagina, often leads to the body's inability to control the overgrowth of fungi that eventually cause inflammation in the area.
Enhancing the normal mechanism of removal of bleeding residues and the immediate restoration of vaginal pH to its normal acidic values can reduce the occurrence of vaginitis after the end of the period.
Indicatively you can combine (scheme for prevention of vaginitis and enhancement of natural balance after period)
Tips:
- Prefer the use of a panty liner with a cotton cover which you change regularly in relation to the tampons
- You can use daily special cleansing fluids for the sensitive area with enhanced composition for protection against microorganisms.
- You can adopt the daily intake of probiotics by mouth through special supplements with lactobacilli to easily and naturally strengthen the flora of the vagina
I often get a recurrence of vaginitis due to fungi. Why is this happening to me? What can I do?
Fungi, although natural colonists of the vagina, very often lead to infections and there are specific reasons that reduce the likelihood of successful reduction and relief from the manifestations of vaginitis. As a result, the recurrence of symptoms of fungal vaginitis is often recorded very soon from the previous episode, which is characterized as a relapse. The main reasons are the development of resistance to the usual medications, the incomplete diagnosis, the self-diagnosis, the non-observance of the treatment regimens, etc.
In any case, the correct and safe diagnosis and treatment is carried out only through the gynecologist after a series of diagnostic tests (colposcopy, vaginal fluid culture, identification of responsible strains, selection of effective active each time, etc.), a practice that is recommended to follow whenever you notice changes in the wider area.
Scrupulous adherence to treatment regimens and the adoption of tactics that directly enhance the local balance and defense of the area are the means to successfully reduce relapses.
Indicatively you can combine (scheme for prevention of vaginitis and enhancement of natural balance)
Tips:
- choose cotton underwear and limit the use of tight synthetic underwear
- avoid the daily use of panty liners
- change your swimsuit immediately and do not sit directly on the sand of the sea
- generally avoid tight clothing and anything that can significantly increase the humidity and temperature of the area
- use daily special cleansing fluids for the sensitive area with enhanced composition for protection against fungi.
Why is it important to get significant amounts of lactic acid in the vagina at any age?
Lactic acid is the factor that shapes the acidic environment in the vagina.
During reproductive age it is released by the lactic acid bacteria of the normal vaginal flora after the metabolism of the glycogen they use as food. The acidic vaginal environment is pleasant and enhances the action of lactobacilli while at the same time limiting the growth of other pathogenic microorganisms.
However, beyond the reproductive age, such as during menopause, maintaining acidic conditions in the vagina can be a means of preventing infections. At this stage of a woman's life, vaginal pH regulators that provide ready-made lactic acid and directly form the required acidity in the vagina can help immediately.
The area of my vagina presents an intense itching, irritation and a burning sensation. What may it be?
Pruritus (itching), irritation and burning sensation are clinical manifestations that can be observed in conditions of different etiology in the vaginal area. They are usually observed in cases of infection of various etiologies that coexist there with increased vaginal secretions with or without odor. The presence of these symptoms without the presence of hypersecretion may be due to the occurrence of vaginal dryness.
In any case, the correct and safe diagnosis and treatment is performed only through the gynecologist after a series of diagnostic tests (colposcopy, vaginal discharge culture, etc.), a practice that is recommended to follow every time you notice changes in the wider area.
MORE FROM MINOR DISCOMFORT

HERBOSEPT
Daily cleansing fluid with natural antibacterial action

EXTRASEPT
Daily cleaning fluid with natural antifungal action

HYDRASEPT
Daily cleansing fluid with moisturizing properties

CHAMOMILE DOUCHE pH 4.2
Vaginal douche with soothing action

ALOE VERA DOUCHE pH 4.2
Vaginal douch with deodorant action

MOIST GEL pH 5.5.
Vaginal gel for hydration & relief from the symptoms of dryness

LACTIC GEL pH 3.8
Vaginal gel for regulating and maintaining vaginal pH

MOIST LONG ACTING GEL pH 3.0
Vaginal gel for long-lasting hydration & relief of dryness symptoms

